Introduction
Nursing documentation and charting refer to the practice of recording a patient’s healthcare information and nursing interventions in a systematic and standardized manner. This documentation can include everything from the patient’s medical history and physical assessment to the care provided by the nursing staff.
Accurate nursing documentation and charting are essential for several reasons. First and foremost, it is a critical tool for ensuring patient safety and continuity of care. By accurately documenting a patient’s condition, healthcare professionals can track changes in their health status over time and provide appropriate treatment and care. Documentation also serves as a legal record of the care provided and can be used as evidence in the event of litigation.
Additionally, nursing documentation and charting are crucial for communication between healthcare professionals. Nurses use this documentation to communicate important information about a patient’s condition and care to other members of the healthcare team, including physicians, therapists, and other nurses. This information sharing helps to ensure that all members of the team are working together to provide the best possible care for the patient.
Overall, accurate nursing documentation and charting are essential for ensuring patient safety, providing effective communication between healthcare professionals, and maintaining legal compliance.
Legal Importance of Nursing Documentation and Charting
Nurses have both legal and ethical obligations to provide high-quality care to their patients. One of the critical components of providing quality care is accurate and complete documentation and charting.
Incomplete or inaccurate nursing documentation can have significant legal implications. If a patient experiences an adverse event or complication, the documentation may be used in legal proceedings to determine if the standard of care was met. If the nursing documentation is incomplete or inaccurate, it may be difficult to determine if appropriate care was provided.
Furthermore, incomplete or inaccurate nursing documentation can lead to risk management and liability issues. In the event of litigation, nurses may be required to provide evidence of their care and interventions. If the documentation is incomplete or inaccurate, this can create doubt about the care provided and increase the likelihood of liability.
On the other hand, thorough and accurate nursing documentation can reduce liability and risk management issues. By documenting all relevant information and interventions, nurses can demonstrate that they provided appropriate care and met the standard of care. This can be an essential defense in legal proceedings and can help to protect both the nurse and the healthcare organization.
In summary, nurses have both legal and ethical obligations to provide high-quality care, which includes accurate and complete nursing documentation and charting. Incomplete or inaccurate documentation can have significant legal implications, including increased risk management and liability issues. Thorough and accurate nursing documentation can reduce liability and demonstrate that appropriate care was provided.
Clinical Importance of Nursing Documentation and Charting
Nursing documentation and charting play a vital role in promoting improved communication and continuity of care. Accurate documentation helps to ensure that all members of the healthcare team are on the same page regarding the patient’s condition, treatment plan, and progress. This can help to prevent errors and misunderstandings and promote better coordination of care.
Additionally, nursing documentation and charting facilitate interdisciplinary communication. Nurses use documentation to communicate important information about a patient’s care and condition to other members of the healthcare team, including physicians, therapists, and other nurses. This interdisciplinary communication helps to ensure that all members of the team are working together to provide the best possible care for the patient.
Nursing documentation and charting also play a critical role in promoting patient safety and quality of care. By accurately documenting a patient’s condition and treatment, nurses can identify potential problems and implement appropriate interventions to prevent adverse events. Documentation can also be used to track a patient’s progress over time and evaluate the effectiveness of interventions.
Furthermore, nursing documentation and charting support evidence-based practice and research. By collecting and documenting data on patient outcomes, healthcare professionals can analyze trends and identify opportunities for improvement. This can lead to the development of evidence-based practices and protocols that improve patient outcomes and quality of care.
In summary, nursing documentation and charting are critical for promoting improved communication and continuity of care, facilitating interdisciplinary communication, promoting patient safety and quality of care, and supporting evidence-based practice and research.
Types of Nursing Documentation and Charting
There are several types of nursing documentation and charting, including:
- Electronic Health Records (EHRs): EHRs are computer-based systems used to record patient information and clinical data. They offer several advantages over traditional paper-based systems, including improved accuracy and efficiency, better communication between healthcare providers, and improved patient safety.
- Narrative charting: Narrative charting involves writing a descriptive account of the patient’s condition and care provided in a chronological order. It can be used to capture the patient’s overall clinical picture, including subjective and objective data, assessments, and interventions.
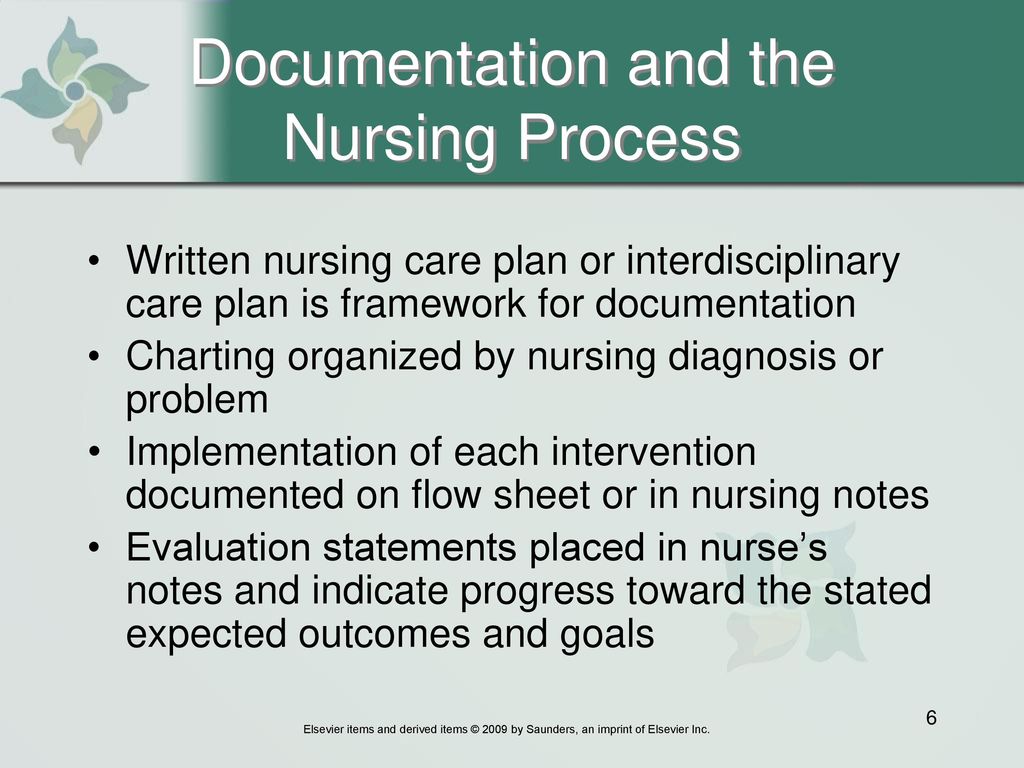
- Problem-oriented charting: Problem-oriented charting involves organizing documentation around the patient’s problems or diagnoses. This method includes four components: problem list, database, plan of care, and progress notes. This approach facilitates systematic and comprehensive documentation and promotes interdisciplinary communication.
- Flow sheets and checklists: Flow sheets and checklists are tools used to document specific types of data, such as vital signs, medications, and procedures. They provide a structured format for documenting information, promote standardization, and reduce the risk of errors.
In summary, there are several types of nursing documentation and charting, including electronic health records, narrative charting, problem-oriented charting, and flow sheets and checklists. Each method has its advantages and disadvantages, and the choice of method depends on the clinical situation and the preferences of the healthcare team.
Conclusion
In conclusion, nursing documentation and charting are critical components of high-quality patient care. Accurate and complete documentation promotes improved communication and continuity of care, facilitates interdisciplinary communication, promotes patient safety and quality of care, and supports evidence-based practice and research.
Nurses have legal and ethical obligations to provide high-quality care, which includes accurate and complete documentation and charting. Incomplete or inaccurate documentation can have significant legal implications, including increased risk management and liability issues. Therefore, it is essential for nurses to prioritize accurate and complete documentation in their daily practice.
Nurses should be encouraged to use appropriate documentation methods that are best suited to the clinical situation and to maintain high standards of documentation throughout the patient’s care journey. By doing so, nurses can help to ensure that patients receive the best possible care and that the healthcare organization can meet legal and regulatory requirements.
See Also-
- Best Crocs For Nurses
- Best Compression Socks For Nurses
- Best Brooks Shoes For Nurses
- Best Bags For Nurses
- Best Backpack For Nurses

